Pulp and Periapical Diseases: Classification, Symptoms, and the Need for Timely Intervention
Pulp and Periapical Diseases: Classification, Symptoms, and the Need for Timely Intervention
Pulp and periapical diseases are critical endodontic conditions requiring precise diagnosis and urgent management to preserve dental health and prevent systemic complications. Below, we outline their classification, clinical manifestations, and why delaying treatment can have severe consequences.
Classification of Pulp and Periapical Diseases
1. Pulpitis (Inflammation of the Dental Pulp)
- Reversible Pulpitis
- Etiology: Caused by shallow caries, traumatic occlusion, or thermal/chemical irritants.
- Symptoms: Transient sensitivity to (hot/cold) or sweet stimuli, resolving promptly after stimulus removal.
- Histology: Mild vascular dilation and inflammatory cell infiltration without irreversible tissue damage.
- Irreversible Pulpitis
- Etiology: Advanced caries, pulpal exposure, or untreated reversible pulpitis.
- Symptoms: Spontaneous pain, prolonged sensitivity to temperature, or referred pain.
- Subtypes: Suppurative pulpitis (purulent exudate) and necrotic pulp (non-vital tissue).

2. Periapical Diseases (Inflammation of Periapical Tissues)
- Chronic Periapical Periodontitis
- Clinical Features: Asymptomatic or mild tenderness; radiographs show periapical radiolucency (e.g., apical granuloma, radicular cyst).
- Acute Periapical Abscess
- Presentation: Severe pain, swelling, tenderness to percussion, and possible fistula formation.
- Complication Risk: Rapid spread to adjacent tissues, leading to cellulitis or Ludwig’s angina.
- Chronic Apical Periodontitis with Symptom Exacerbation
- Triggers: Immune compromise or reinfection; presents with acute symptoms on a chronic lesion.
Why Treatment Can't Wait: The Urgency of Intervention
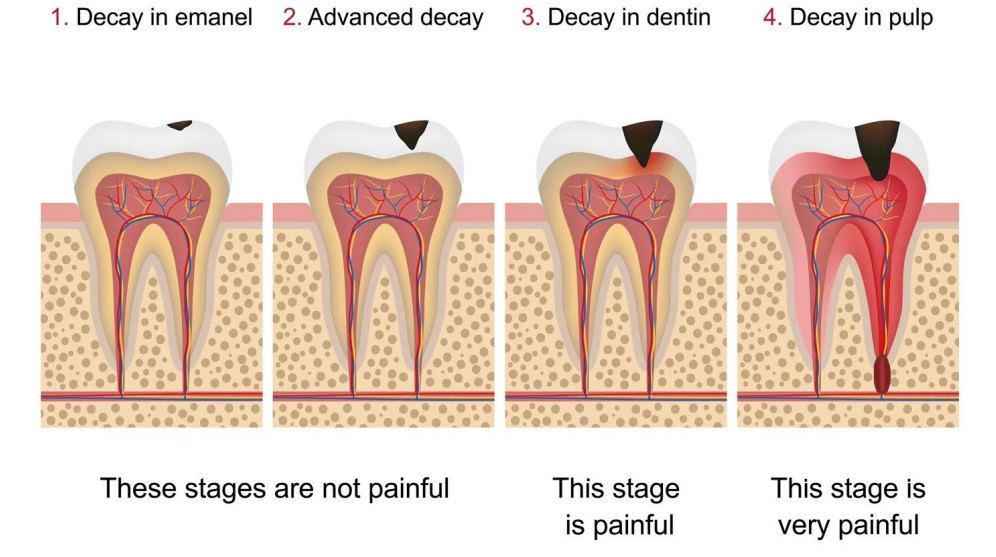
1. Disease Progression and Tooth Loss
- Untreated pulpitis progresses to pulpal necrosis, releasing bacteria and toxins into the periapical space. This triggers osteoclastic activity, leading to periapical bone resorption and eventual tooth instability.
- Data Insight: 87% of untreated irreversible pulpitis cases develop apical periodontitis within 6–12 months (Journal of Endodontics, 2023).
2. Systemic Health Risks
- Periapical infections can spread to the maxillofacial region or bloodstream, causing life-threatening conditions like cavernous sinus thrombosis or sepsis, particularly in immunocompromised patients.
3. Treatment Complexity Escalates with Delay
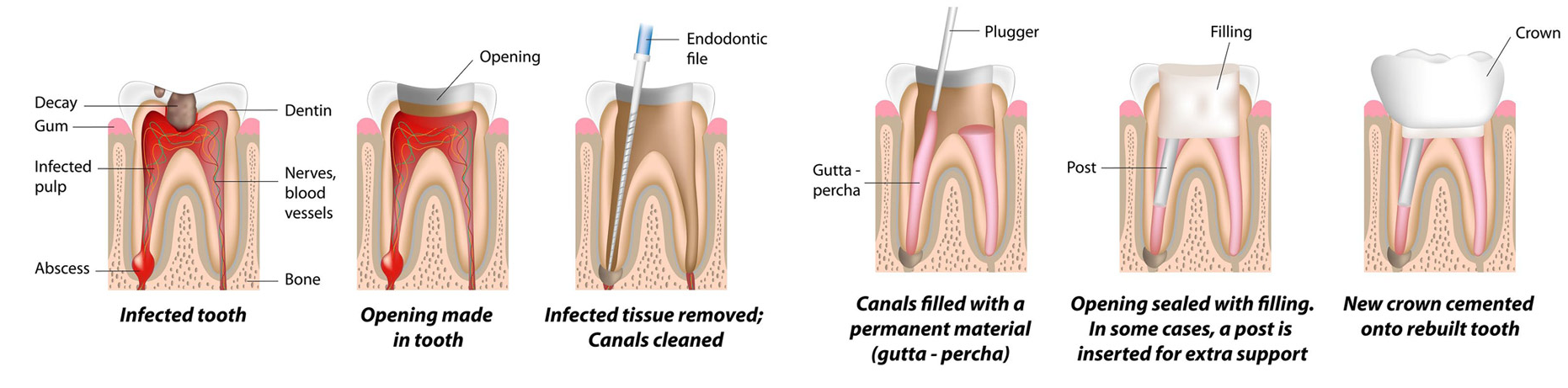
- Early-stage reversible pulpitis may respond to indirect pulp capping or pulpotomy.
- Advanced cases require root canal therapy (RCT), and severe apical lesions may need surgical intervention (apicoectomy). Neglect can lead to tooth extraction as the last resort.

Key Takeaways for Patients & Practitioners
- Early Diagnosis Saves Teeth: Regular dental exams with digital radiography enable timely detection of subtle pulpal/periapical changes.
- Pain is a Late Symptom: Even asymptomatic radiolucencies indicate active infection—do not dismiss "silent" lesions.
- Treatment Gold Standard: RCT remains the most effective intervention, preserving natural dentition when performed within the first signs of irreversible pulpitis.
Act Now to Preserve Oral Health
Pulp and periapical diseases follow a predictable progression: prevention > early intervention > complex treatment > extraction. Don’t let delay compromise prognosis. If you experience prolonged sensitivity, swelling, or tooth tenderness, seek endodontic evaluation immediately.