Guided Bone Regeneration (GBR) in Dental Implantology
Guided Bone Regeneration (GBR) in Dental Implantology




I. Core Purposes of Guided Bone Regeneration (GBR) in Dental Implant Bone Grafting
Guided Bone Regeneration (GBR) is a pivotal technique in implant bone grafting. Its fundamental principle is to utilize a biomembrane barrier to isolate gingival epithelial cells and fibroblasts, thereby creating an exclusive space for osteoblast proliferation and growth, and ultimately achieving precise repair and regeneration of bone tissue. The specific purposes are as follows:
Precise Repair of Bone Defects
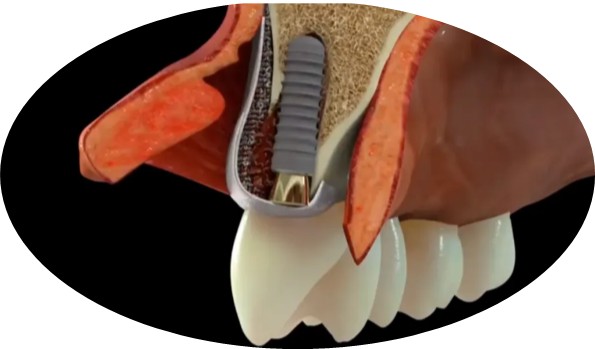
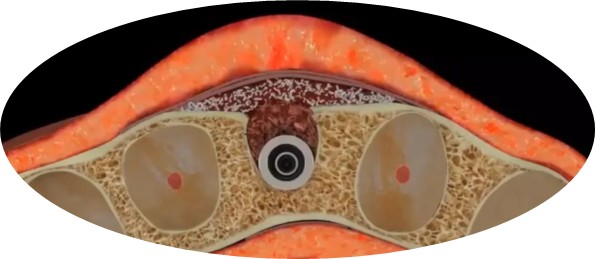
For localized bone defects such as alveolar bone concavities and insufficient bone width caused by post-extraction bone resorption, as well as defects induced by trauma or periodontal disease, GBR combines barrier membranes with bone graft materials (autogenous bone, xenogeneic bone or synthetic bone substitutes) to guide the directional growth of new osteoblasts in the defect area, restore the normal morphology and dimensions of the alveolar bone, and meet the bone volume requirements for implant placement.
Ensuring Osseointegration of Dental Implants
The barrier membrane prevents soft tissue cells from invading the bone defect area and interfering with bone healing. Meanwhile, the bone graft material acts as a scaffold to support the gradual replacement of the graft material by newly formed bone tissue. This ultimately results in a healthy bone bed that is tightly integrated with the implant, significantly enhancing the primary stability and long-term success rate of the implant.
Maintaining Aesthetic Contour of Peri-implant Soft Tissues
Sufficient newly formed bone tissue can effectively support the gingival papillae and mucosa around the implant, prevent postoperative gingival atrophy and collapse, maintain a harmonious gingival line between the implant and natural teeth, and achieve dual restoration of function and aesthetics.
II. Brief Post-Implantation Precautions (Including GBR Procedure)
Since GBR involves the use of barrier membranes and bone graft materials, it requires higher standards for postoperative healing. Patients should adhere to the following precautions:
(I) Short-term Postoperative Care (1–2 Weeks, Critical Healing Period)
Hemostasis and Prevention of Membrane Exposure
Bite on the hemostatic gauze roll for 30–45 minutes after surgery. For 24 hours postoperatively, refrain from rinsing the mouth, spitting, or forceful suction to prevent blood clot detachment, which could lead to bleeding or dry socket.
If persistent oozing occurs at the surgical site, contact your dentist promptly for follow-up; do not attempt self-treatment.
Management of Swelling and Pain Relief with Positioning Guidance
Apply cold compresses to the facial area corresponding to the surgical site within 48 hours after surgery (15 minutes per session, with 1-hour intervals) to reduce swelling and pain.Switch to warm compresses after 48 hours to promote hematoma resolution.
Elevate the head during sleep to reduce congestion at the surgical site and alleviate swelling discomfort.
Dietary and Lifestyle Restrictions
Consume cool, lukewarm liquid foods (e.g., chilled milk, yogurt, fruit juice) within 24 hours postoperatively. Transition to semi-liquid foods (e.g., porridge, mashed noodles) within 1week, and avoid chewing on the surgical side throughout this period.
Abstain from smoking and alcohol for at least 2 weeks postoperatively (smoking and alcohol consumption can disrupt blood clot formation, inhibit osteoblast proliferation, and significantly increase the risk of membrane exposure and infection). Avoid spicy, hard, or overheated foods.
Oral Hygiene and Medication Compliance
Do not brush your teeth within 24 hours after surgery. After this period, use a soft-bristled toothbrush to gently clean non-surgical areas. Rinse the surgical area with 0.12% chlorhexidine gluconate mouthwash twice daily for 1 minute per rinse, for 1–2 weeks as directed by your dentist. Do not use dental floss or water flossers near the surgical site.
Strictly follow the dentist’s instructions for taking antibiotics (e.g., amoxicillin + metronidazole, ensure no allergies) and analgesics. Do not discontinue medication or adjust dosages without authorization.
(II) Medium-term Postoperative Recovery (2–6 Months, Critical Period for Bone Regeneration)
Avoidance of External Stimuli
Do not touch the gingiva at the surgical site with your hands, protect the implant area from impact, and refrain from biting hard objects to prevent displacement of the barrier membrane or impairment of the implant’s primary stability.
Enhanced Oral Hygiene Maintenance
Maintain thorough oral hygiene in non-surgical areas by using dental floss and water flossers to clean interdental spaces, preventing plaque accumulation that could lead to periodontal issues. For the surgical area, follow the dentist’s instructions strictly for cleaning; resume normal cleaning protocols only after the barrier membrane has been covered by soft tissue.
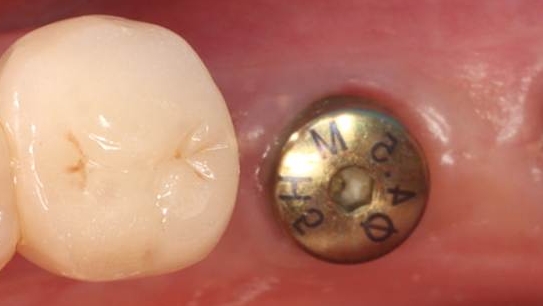
Regular Follow-up Visits for Healing Monitoring
Return for suture removal 1 week after surgery, during which the dentist will inspect the membrane position and bone healing progress. Subsequent follow-up appointments (at 1 month and 3 months) will include radiographic examinations to evaluate new bone formation and timely detect complications such as membrane exposure or infection.
(III) Long-term Postoperative Maintenance (After 6 Months, Following Prosthetic Restoration)
Daily Cleaning and Professional Maintenance
After prosthetic restoration of the implant, clean the implant surface with a soft-bristled toothbrush daily, and use dental floss or interdental brushes to clean adjacent surfaces. Undergo professional scaling and peri-implant examinations every 6–12 months to remove dental calculus and plaque.
Occlusal and Functional Management
Avoid biting hard objects (e.g., nuts, bones) with the implant. If occlusal pain or implant mobility occurs, seek prompt dental attention for occlusal adjustment to prevent peri-implantitis or bone resorption.

